The following information has been written by Dr Camilla Janssen for New Forest Primary Care Network, being used with permission.
The menopause is a natural part of ageing that usually occurs between 45 and 55 years of age, as a woman's oestrogen levels decline. In the UK, the average age for a woman to reach the menopause is 51. The perimenopausal stage normally lasts for a few years leading up to this.
You are thought to be “post-menopausal” when you have had a year since your last period. (But you are only able to know this if you are not on any hormones or contraception that may affect your periods).
If you have read the information below and you feel HRT would be beneficial:
|
Symptoms may include some or all of the below and can be intermittent initially:
|
|

We typically diagnose menopause from symptoms alone and don't need to do blood tests.
When should you start on HRT?
It is beneficial to start HRT when menopausal symptoms impact on your home, work, social or sex life and you deem that the benefits of HRT will outweigh the risks. This may start a few years before your periods actually stop. See this link for more information. Is it ever too late to start HRT?
If you have had a Surgical Menopause - i.e. your ovaries have been removed surgically, then you should replace the hormones that your body is no longer producing until the time a natural menopause would occur at the earliest -i.e. 51yrs. There are no increased risks related to HRT as you are replacing the hormones that your body would otherwise produce.
Primary Ovarian Insufficiency (POI) also known as Premature Menopause, affects up to 1 in 100 women and this is when your periods stop before the age of 40. It means your ovaries are not working well and the lack of hormones cause many associated troublesome symptoms and health conditions if left untreated. It is important to replace the hormones that your body is no longer producing until the age of natural menopause at the earliest i.e. 51yrs old. There are no increased risks related to HRT before age of natural menopause, as you are replacing the hormones that your body would otherwise produce. Daisy Network is dedicated to providing information and support to women diagnosed with Premature Ovarian Insufficiency.
What are the Benefits and Risks?
This advice has fluctuated over the years and has caused considerable confusion. More recently published findings show that although not entirely risk free, it remains that HRT is the most effective solution for the relief of menopausal symptoms, and it also works to prevent future diseases that can be triggered or exacerbated by low hormone levels. Link to Women's Health Concerns Fact Sheet on the Risks and Benefits of HRT.
BENEFITS
- Reduction of the symptoms of the Menopause with resultant improved of quality of life.
- Prevention of osteoporosis.
- Protection against heart disease in certain age groups. The risk of heart disease increases with age, and it is the leading cause of death for women. HRT has been shown to reduce the risk of women developing heart disease by 30-50% if started within 10 years of menopause.
- Reduces the risk of developing type 2 diabetes, bowel cancer, dementia, and depression suggested in some studies.
RISKS
- Breast Cancer is more complex, and many women worry about this in relation to HRT. Essentially 1 in 7 women born after 1960 will experience breast cancer at some point in their lives. Taking HRT makes very little difference to this. If you take oestrogen only HRT (only applicable if you have no uterus or if you have a Mirena coil) you have a reduction in risk of being diagnosed or dying from breast cancer. If you take combination HRT you have a slight increased risk of being diagnosed with breast cancer but no increased risk of dying from breast cancer. In trials, obesity or drinking 2 glasses of wine a night posed a bigger risk factor than being on HRT in respect to the risk of getting breast cancer. Click here to see British Menopause Society info and chart and Newson Health link.
- Blood Clots - older studies have suggested an increased clotting link with older forms of oral HRT, this risk is not evident if newer formulations of HRT are taken through the skin. Click here to read about Menopause and Clots.
Other personal characteristics can play a bigger part than HRT in increasing the risk for many conditions such as Breast Cancer, Stroke and Venous Thromboembolic events such as a Deep Vein Thrombosis or Pulmonary Embolus. These include Obesity, Smoking and Alcohol. It is important to manage these risks independently. Click on this infographic to see the comparison of lifestyle risk factors versus Hormone Replacement Therapy (HRT) treatment and the risk of Breast Cancer
Many lifestyle factors can improve the symptoms of the menopause. A lower carbohydrate diet is a good way to stabilise blood sugars and help with menopausal symptoms as well as addressing obesity and hence other risk factors. Sleep, physical exercise, mental wellbeing, with a healthy out look on life, have a huge impact on how we feel. We suggest looking at our lower carbohydrate pages link here as well as all the health and wellbeing resources embedded in this website. It is worth optimising how you are running your body before adding medications.
Non hormonal prescribed HRT alternatives options to address the menopausal symptoms - Prescribable Non-HRT and What are the alternatives to HRT?.
Common Side effects of HRT - These are common in the first 3 months of starting HRT and tend to improve with time.
- Breast tenderness
- Change in skin/acne
- Bloating, mood swings
Bleeding on HRT - Common in first 4 – 6 months of any new HRT regime. It typically does not indicate anything abnormal and usually settles with time. If it persists for more than 4-6 months, then please discuss with a doctor. We can tweak your hormone combination to improve things and we may need to investigate to ensure nothing else is causing the bleeding at this point.
Body Identical vs Bioidentical - Body identical HRT are medicines that have been subjected to safety testing and quality control and are regulated by the Medicines Regulatory Agency. This is the HRT we prescribe in the NHS. It comes as a transdermal preparation (i.e. one that you take via the skin) either as a gel that you rub on daily or as a patch that you change twice a week. Uterogestan is the body identical progesterone. Bioidentical HRT products are unregulated and is a term used for products which are marketed as being "natural" or "individualised" or "customised" for women. These products are unregulated by the Medicines Regulatory Agency and are unlicensed. They have not been subject to the same safety testing or quality control as the regulated HRT products in body identical HRT. The use of bioidentical compounded hormones is not recommended by the British Menopause Society.
Natural Alternatives to HRT - beware, natural doesn't mean safe - arsenic is natural. This Menopause Matters website has wealth of information on menopause, including information on natural alternatives to HRT. Most GPs are not trained in this area and are not able to prescribe these, so you may have to do your own research on these products.
How long should you continue with HRT? - HRT should be continued for as long as benefits of symptom control and improved quality of life outweigh any risks, and there is no arbitrary limit for duration of HRT use. Benefits from HRT re heart disease, bones and brain etc only continue with ongoing use.
Peoples menopausal symptoms vary from none at all to lifelong debilitating symptoms. Menopausal symptoms naturally improve with time in the majority and the minority will get lifelong flushing and symptoms. Symptoms are often worse during the perimenopausal years and improve with time. The symptoms tend to subside as your body gets used to lower oestrogen levels and as you get older you may need a lower dose of HRT or none at all.
It is reasonable to continue HRT long term or use it for 2-5 years and at then consider reducing the oestrogen dose or trialling without HRT at this point and see how your body responds. You can either stop abruptly (expect some initial symptoms) or gradually reduce over time. There is no long-term differences in the outcome between stopping abruptly versus gradually decreasing your dose. If you do stop abruptly, it is normal to have some initial symptoms due to the relative lack of oestrogen, but this should settle over time – over a few weeks to a couple of months, so please do expect this.
Please ensure that you participate in regular breast and cervical screening programmes.
Once started on HRT, we would suggest a follow up with your GP in 3 months’ time with an up-to-date blood pressure reading. Once things are stabilised, an annual review, including and up to date blood pressure, is perfectly appropriate.
If you get new bleeding once established on HRT for more than 6 months, please discuss this with your doctor, as this usually needs investigating.
USEFUL WEBSITES and RESOURCES
The British Menopause Society (BMS) is also a good source of reliable information. BMS tools for clinicians has a useful range of resources that summarise the NICE Guideline, provide guidance on HRT prescribing and other treatment options, and to clarify some of the most common myths and misconceptions of menopause.
Newson Health is a private Menopause and Wellbeing Centre. There is a wealth of information on its website including a comprehensive resources page which features fact sheets, booklets and podcasts on many different areas of menopause.
Menopause Matters website has wealth of information on menopause, including information on natural alternatives to HRT.
Primary Care Women's Health Forum has a wealth of information including patient information leaflets as per link.
Balance app allows you to track your symptoms, access personalised expert content, download a Health Report©, share stories in the community and lots more.
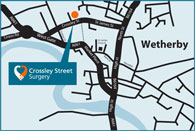
Leeds Centre for Women's Health Menopause Care in Leeds
The Menopause Clinic @ Meanwood Testosterone Therapy